We live in a rather pleasant time in history where biotechnology is blossoming, and people in general don’t appear to be using it for weapons. If the rest of human existence can carry on like this, that would be great. In case it doesn’t, we’re going to need back-up strategies.
Here, I investigate some up and coming biological innovations with a lot of potential to help us out here. I kept a guiding question in mind: will biosecurity ever be a solved problem?
If today’s meat humans are ever replaced entirely with uploads or cyborg bodies, biosecurity will be solved then. Up until then, it’s unclear. Parasites have existed since the dawn of life – we’re not aware of any organism that doesn’t have them. When considering engineered diseases and engineered defenses, we’ve left the billions-of-years-old arms race for a newer and faster paced one, and we don’t know where an equilibrium will fall yet. Still, since the arrival of germ theory, our species has found a couple broad-spectrum medicines that have significantly reduced threat from disease: antibiotics and vaccines.
What technologies are emerging now that might fill the same role in the future?
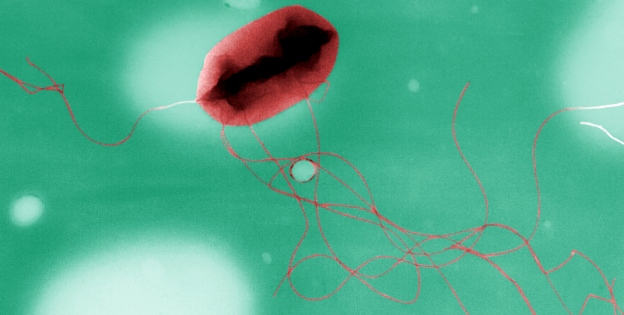
Phage therapy
What it is: Viruses that attack and kill bacteria.
What it works against: Bacteria.
How it works: Bacteriophage are bacteria-specific viruses that have been around since, as far as we can tell, the dawn of life. They occur frequently in nature in enormous variety – it’s estimated that for every bacteria on the planet, there are 10 phages. If you get a concentrated stock of bacteriophage specific to a given bacteria, they will precisely target and eliminate that strain, leaving any other bacteria intact. They’re used therapeutically in humans in several countries, and are extremely safe.
Biosecurity applications: It’s hard to imagine even a cleverly engineered bacteria that’s immune to all phage. Maybe if you engineered a bacteria with novel surface proteins, it wouldn’t have phage for a short window at first, but wait a while, and I’m sure they’ll come. No bacteria in nature, as far as we’re aware, is free of phage. Phage have been doing this for a very, very long time. Phage therapy is not approved for wide use in the US, but has been established as being safe and quite effective. A small dose of phage can have powerful impacts on infection.
Current constraints: Lack of research. Very little current precedent for using phage in the US, although this may change as researchers hunt for alternatives to increasingly obsolete antibiotics.
Choosing the correct phage for therapeutics is something of an art form, and phage therapy tends to work better against some kind of infection than others. Also, bacteria will evolve resistance to specific phages over time – but once that happens, you can just find new phages.
DRACO
What it is: Double RNA Activated Capsase Oligomerizer. An RNA-based drug technology recently invented at MIT.
What it works against: Viruses. (Specifically, double-stranded RNA, single-stranded RNA, and double-stranded DNA (dsRNA, ssRNA, and dsDNA), which is most human viruses.)
How it works: DsDNA, dsRNA, and ssRNA virus-infected cells each produce long sequences of double-stranded RNA at some point while the virus replicates. Human cells make dsRNA occasionally, but it’s quickly cleaved into little handy little chunks by the enzyme Dicer. These short dsRNAs then go about, influencing translation of DNA to RNA in the cell. (Dicer also cuts up incoming long dsRNA from viruses.)
DRACO is a fusion of several proteins that, in concert, goes a step further than Dicer. It has two crucial components:
- P that recognizes/binds viral sequences on dsRNA
- P that triggers apoptosis when fused
Biosecurity applications: The viral sequences it recognizes are pretty broad, and presumably, it wouldn’t be hard to generate addition recognition sequences for arbitrary sequences found in any target virus.
Current constraints: Delivering engineered proteins intracellularly is a very new technology. We don’t know how well it works in practice.
DRACO, specifically, is extremely new. It hasn’t actually been tested in humans yet, and may encounter major problems in being scaled up. It may be relatively trivial for viruses to evolve a means of evading DRACO. I’m not sure that it would be trivial for a virus to not use long stretches of dsRNA. It could, however, evolve not to use targeted sequences (less concerning, since new targeting sequences could be used), inactivate some part of the protein (more concerning), or modify its RNA in some way to evade the protein. Even if resistance is unlikely to evolve on its own, it’s possible to engineer resistant viruses.
On a meta level, DRACO’s inventor made headlines when his NIH research grant ran out, and he used a kickstarter to fund his research. Lack of funding could end this research in the cradle. On a more meta level, if other institutions aren’t leaping to fund DRACO research, experts in the field may not see much potential in it.
Programmable RNA vaccines
What it is: RNA-based vaccines that are theoretically creatable from just having the genetic code of a pathogen.
What it works against: Just about anything with protein on its outside (virus, bacteria, parasite, potentially tumors.)
How it works: An RNA sequence is made that codes for some viral, bacterial, or other protein. Once the RNA is inside a cell, the cell translates it and expresses the protein. Since it’s not a standard host protein, the immune system recognizes and attacks it, effectively creating a vaccine for that molecule.
The idea for this technology has been around for 30-odd years, but the MIT team that discovered this were the first to package the RNA in a branched, virus-shaped structure called a dendrimer (which can actually enter and function in the cell.)
Biosecurity applications: Sequencing a pathogen’s genome should be quite cheap and quick once you get a sample of it. An associate professor claims that vaccines could be produced “in only seven days.”
Current constraints: Very new technology. May not actually work in practice like it claims to. Might be expensive to produce a lot of it at once, like you would need for a major outbreak.
Chemical antivirals
What it is: Compounds that are especially effective at destroying viruses at some point in their replication process, and can be taken like other drugs.
What it works against: Viruses
How it works: Conventional antivirals are generally tested and targeted against specific viruses.
The class of drugs called thiazolides, particularly nitazoxanide, is effective against not only a variety of viruses, but a variety of parasites, both helminthic (worms) and protozoan (protists like Cryptosporidum and Giardia.) Thiazolides are effective against bacteria, both gram positive and negative (including tuberculosis and Clostridium difficile). And it’s incredibly safe. This apparent wonderdrug appears to disrupt creation of new viral particles within the infected cell.
There are others, too. For instance, beta-defensin P9 is a promising peptide that appears to be active against a variety of respiratory viruses.
Biosecurity applications: Something that could treat a wide variety of viruses is a powerful tool against possible threats. It doesn’t have to be tailored for a particular virus- you can try it out and go.
Current constraints: Discovery of new antibiotics has slowed down. Antivirals are a newer field, but the same trend may hold true.
Also, using a single compound drastically increases the odds that a virus will evolve resistance. In current antiviral treatments, patients are usually hit with a cocktail of antivirals with different mechanisms of action, to reduce the chance of a virus finding resistance of them.
Space for finding new antivirals seems promising, but they won’t solve viruses any more than antibiotics have solved bacterial infections – which is to say, they might help a lot, but will need careful shepherding and combinations with other tactics to avoid a crisis of resistance. Viruses tend to evolve more quickly than bacteria, so resistance will happen much faster.
Gene drives
What it is: Genetically altering organisms to spread a certain gene ridiculously fast – such as a gene that drives the species to extinction, or renders them unable to carry a certain pathogen.
What it works against: Sexually reproducing organisms, vector-borne diseases (with sexually reproducing vectors.)
How it works: See this video.
Biosecurity applications: Gene drives have been in the news lately, and they’re a very exciting technology – not just for treating some of the most deadly diseases in the world. To see their applications for biosecurity, we have to look beyond standard images of viruses and bacteria. One possible class of bioweapon is a fast-reproducing animal – an insect or even a mouse, possibly genetically altered, which is released into agricultural land as a pest, then decimates food resources and causes famine.
Another is release of pre-infected vectors. This has already been used as a biological weapon, including Japan’s infamous Unit 731, which used hollow shells to disperse fleas carrying the bubonic plague into Chinese villages. Once you have an instance of the pest or vector, you can sequence its genome, create a genetic modification, and insert the modification along with the gene drive sequences. This can either wipe the pest out, or make it unable to carry the disease.
Current constraints: A gene drive hasn’t actually been released into the wild yet. It may be relatively easy for organisms to evolve strategies around the gene drive, or for the gene drive genes to spread somehow. Even once a single gene drive, say, for malaria, has been released, it will probably have been under deep study for safety (both directly on humans, and for not catastrophically altering the environment) in that particular case – the idea of a gene drive released on short notice is, well, a little scary. We’ve never done this before.
Additionally, there’s currently a lot of objection and fears around gene drives in society, and the idea of modifying ecosystems and things that might come into contact with people isn’t popular. Due to the enormous potential good of gene drives, we need to be very careful about avoiding public backlash to them.
Finding the right modification to make an organism unable to carry a pathogen may be complicated and take quite a while.
Gene drives act on the pest’s time, not yours. Depending on the generation time of the organism, it may be quite a while before you can A) grow up enough of the modified organism to productively release, and B), wait while the organism replicates and spreads the modified gene to enough of the population to have an effect.
Therapeutic antibodies
What it is: Concentrated stocks of antibodies similar to the ones produced in your own body, specific to a given pathogen.
What it works against: Most pathogens, some toxins, cancers.
How it works: Antibodies are proteins produced by B-cells as part of the adaptive immune system. Part of the protein attaches to a specific molecule that identifies a virus, bacteria, toxin, etc.. The rest of the molecule acts as a ‘tag’ – showing other cells in the adaptive immune system that the tagged thing needs dealt with (lysed, phagocytosed, disposed of, etc.)
Biosecurity applications: Antibodies can be found and used therapeutically against a huge variety of things. The response is effectively the same as your body’s, reacting as though you’d been vaccinated against the toxin in question, but it can be successfully administered after exposure.
Current constraints: Currently, while therapeutic antibodies are used in a few cases like snake venom and tumors, they’re extremely expensive. Snake antivenom is taken from the blood serum of cows and horses, while more finicky monoclonal therapeutics are grown in tissue culture. Raising entire animals for small amounts of serum is pricey, as are the nutrients used for tissue culture.
One possible answer is engineering bacteria or yeast to produce antibodies. These could grow antibodies faster, cheaper, and more reliably than cell culture. This is under investigation – E. coli doesn’t have the ability to glycosylate proteins correctly, but that can be added in with genetic engineering, and anyways, yeasts can already do that. The promise of cheap antibody therapy is very exciting, and more basic research in cell biology will get us there faster.

Love your name by the way.
LikeLike
I had had some background concern about this and this post was somewhat reassuring! Regarding phages, it seems like it would be wise for defensive biotech researchers to proactively attempt to create bacteria that have different kinds of novel surface proteins (yet aren’t dangerous) for the purpose of creating a context for the evolution of adequate phage that will be able to tackle potential dangerous bacteria.
LikeLike